Waiting for the Weekend: Is the NFL Really in Trouble This Time? 5
A recent study of the brains of former NFL players showed almost all had some level of brain trauma.
For the last year or more, it seems every time there is a negative story about the NFL, it prompts the obligatory question of whether that particular issue will be the proverbial “straw that broke the camel’s back” and signal the start of the decline for the financial and popularity juggernaut.
Whether it be declining television ratings, continued off-the-field incidents by players, the perception by many that the game isn’t as physical as in past, the abandonment of long-time NFL cities in St. Louis, San Diego and Oakland, the general unpopularity of Roger Goodell and the New England Patriots or a number of other “negative” stories or events, they all seem to just roll off the back of the NFL as overall revenues continue to increase to levels envied by most governments or for-profit businesses.
However, news that came out this week may over time be the one story that the NFL cannot easily shake.
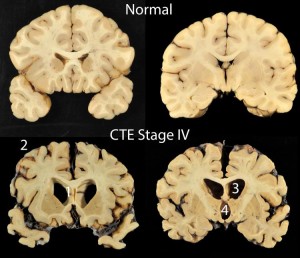
A scientific study published this week in the medical journal JAMA looked at the brains of 202 deceased former high school, college and professional football players. Amongst those former players, 177, including 110 of the 111 former NFL players, were diagnosed as having CTE (Chronic Traumatic Encephalopathy).
CTE is a degenerative brain disease most often found in athletes, military veterans, and others with a history of repetitive brain trauma. To create CTE, a protein called Tau forms clumps that slowly spread throughout the brain, killing brain cells. Studies have found CTE in people as young as 17, but symptoms most typically don’t begin appearing until years after the initial head impacts.
Early symptoms of CTE affect a patient’s mood and behavior. Some common changes often include impulse control problems, aggression, depression, and paranoia.
As the disease progresses, it is typical for patients to experience problems with thinking and memory, including memory loss, confusion, impaired judgment, and eventually progressive dementia. Cognitive symptoms tend to appear later than mood and behavioral symptoms, and often first appear when the patient is in their 40s or 50s. Patients may exhibit one or both symptom clusters and the symptoms may often worsen with time (even if the patient suffers no additional head impacts). In other cases, symptoms may be stable for years before worsening. Read the rest of this entry →